Bedsores or Pressure Ulcers

What are bedsores?
Also known as pressure ulcers, pressure injuries, pressure sores, or decubitus ulcers, form from prolonged pressure on various parts of the body. While they can occur anywhere, they are more likely to develop on bony areas such as the elbows, knees, heels, tailbone, and ankles. Bedsores can happen when a person is bedridden, sitting in a wheelchair for a long period, or otherwise immobile, unconscious, or unable to sense pain.
Most sores heal with treatment, but some never heal completely. Without treatment, the sores can eventually lead to potentially fatal complications. You can take steps to help prevent bedsores and help them heal.
What causes bedsores?
A bedsore is developed when the blood vessels supplying the skin are obstructed for more than 2-3 hours. It typically starts as a red, painful area which then turns purple. Without treatment, the skin can break open and become infected.
Below are 3 primary contributing factors for bedsores:
- Pressure. Too much pressure on any area of your body can prevent blood from flowing to that region. Blood flow is how oxygen and other nutrients are delivered to cells, so without it, tissue will be damaged and might eventually die. People with restricted mobility often have this kind of pressure in areas without much padding or fat, such as the spine, tailbone, shoulder blades, hips, heels and elbows.
- Friction. Friction is caused when the skin rubs against another surface, like clothing or bedding. If the skin is already fragile, this increased friction can make it more susceptible to injury—particularly if the skin is moist.
- Shear. Shear forces are generated when two surfaces move in the opposite direction. For example, when you sit upright in bed and then lower yourself back down, your skin might stay in place as your tailbone moves downward.
What are the symptoms (stages) of bedsores?
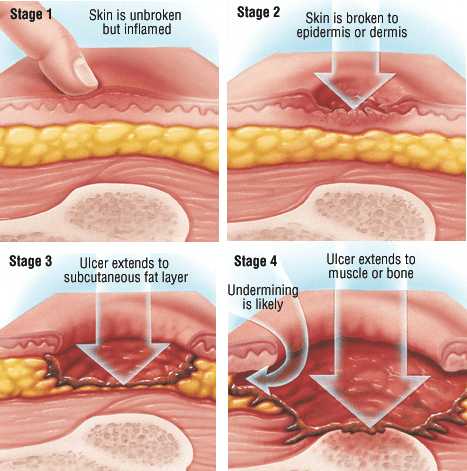
Bedsores are divided into 4 stages, from least severe to most severe. These are:
Stage I: A reddened, painful area on the skin that does not turn white (blanch) when pressed. This is a sign that a pressure ulcer may be forming. The skin may be warm or cool, firm or soft.
Stage II: The skin blisters or forms an open sore. The area around the sore may be red and irritated.
Stage III: The skin now develops an open, sunken hole called a crater or ulcer. The tissue below the skin is damaged. You may be able to see body fat in the ulcer.
Stage IV: The pressure ulcer has become so deep that there is damage to the muscle and bone, and sometimes to tendons and joints.
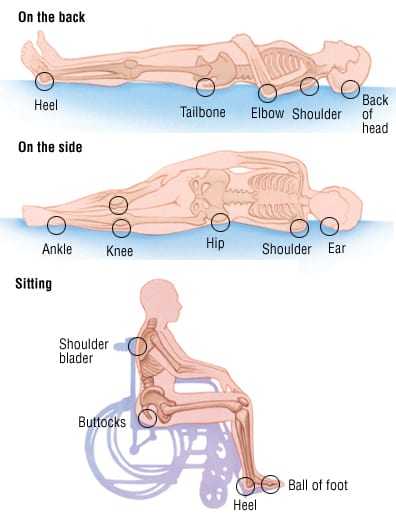
Common areas on the body at risk of developing Bedsores
For wheelchair-bound individuals, bedsores often occur on the skin over the following sites:
- Tailbone or buttocks
- Shoulder blades and spine
- Backs of arms and legs where they rest against the chair
For bedridden individuals, bedsores may happen on:
- Back or sides of the head
- Shoulder blades
- Hip, lower back or tailbone
- Heels, ankles and skin behind the knees
Who is at risk for developing pressure injuries?
- People with a limited amount of mobility or a total inability to move
- Prosthetic (artificial) limb users
- People with a loss of sensation
- Poor nutrition and hydration.
- The elderly
Can bedsores be prevented?
To avoid bedsores, check the skin daily for red spots (the earliest sign of skin damage), paying special attention to bony areas. Other ways to prevent bedsores or keep existing sores from getting worse are:
- Turning and repositioning the patient every 1-2 hours on the bed
- Change position every 15-30 minutes while sitting
- Use a reclining wheelchair that can recline the body and elevate the legs
- Use pressure-relieving cushions on wheelchairs and ripple mattresses for beds
- Use foam wedges and pillows while sleeping sideways
- Keep skin clean and dry and inspect daily for signs
- Eat a healthy and balanced diet
What are the complications of bedsores?
If a bedsore is not treated properly, it can take days or even years to heal. If left untreated, there will be long-term consequences such as Cellulitis (Skin), Osteomyelitis (Bone), Bacteremia (Blood), Meningitis (Brain and Spinal Cord), and Endocarditis (Heart) are imminent. These life-threatening infections that could be fatal.
When should I call the doctor?
If you believe you are at a higher risk of developing pressure ulcers, it's best to speak with a healthcare professional. It's also essential to seek an accurate diagnosis and start formal treatment immediately if you already have a pressure ulcer—this will help avoid additional complications from occurring.
Where to buy high quality medical equipment and supplies?
Visit our online store at www.neolee.com.my
Customer enquiries:
Phone: (KL) 03-92129402 / (JB) 07-5190350
Email: general.enquiry@neolee.com.my
or Visit our showroom
For more stories like this, join our Facebook community on Facebook
Need help with your order? chat with us here via Whatsapp
Oct 27,2022